SCRAM™
Structured CRitical Airway Management
“Our vision is to enhance the performance of emergency airway management by promoting Safe, Well Governed Emergency Anaesthesia and Tracheal intubation.”
The SCRAM™ Story
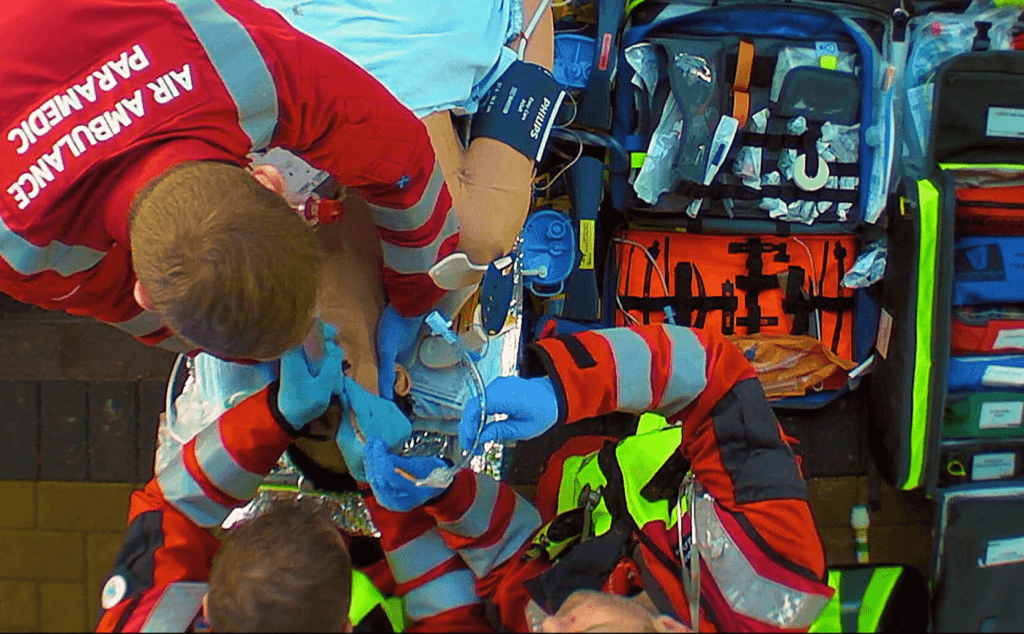
Emergency Anaesthesia with oral tracheal intubation is the technique of choice to manage critically ill or injured patients who cannot maintain their airway or achieve adequate ventilation1,2.
Emergency Airway management occurring outside the operating theatre is associated with increased morbidity and mortality3,4. Poor planning, absent or unfamiliar equipment and interrupted workflow are all potential contributory factors 2,3,4.
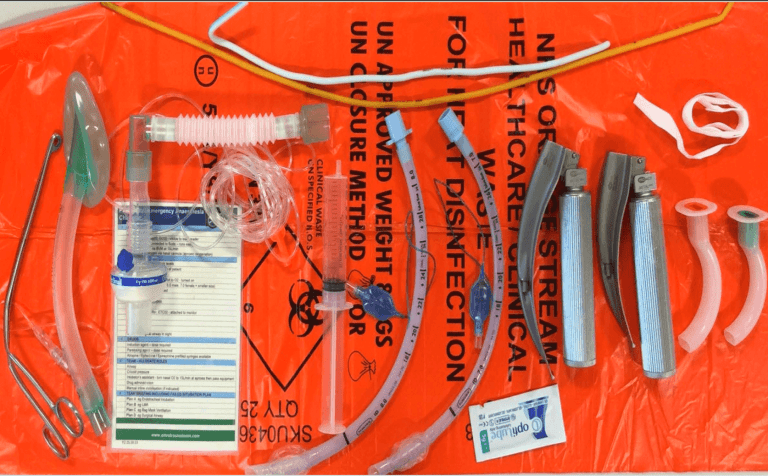
Preparing for Emergency Anesthesia and tracheal intubation involves establishing an equipment “kit dump” and drugs for the intervention. Various methods exist, one such method which is well described and employed by many teams is to setup on a clinical waste bag (fig 1) and another example (fig 2). However, in practice I found this method to be vulnerable to the elements and knew it could be improved upon, which is where the idea of having a kit dump in a bag started to evolve. However, I didn’t want to create just another airway bag that carried / stored kit it needed to add value.
What would make this difference and how would we work this out?
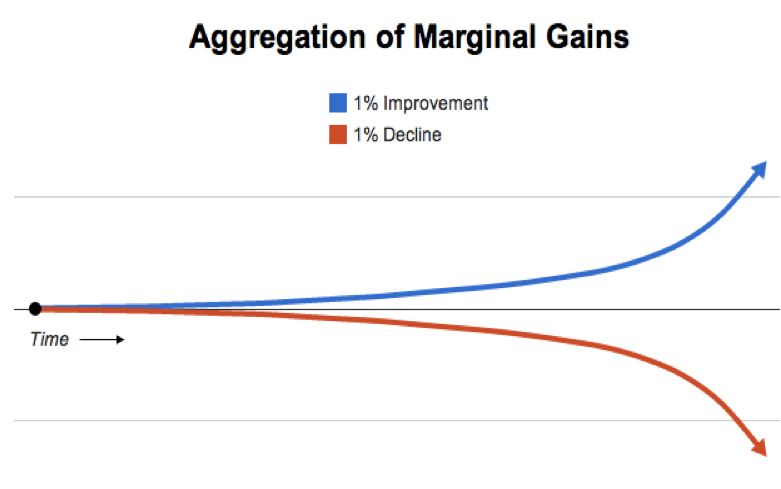
So, using the concept of “aggregation of marginal gains”5 (Fig 3) (utilised by high performance teams to optimize performance) and by breaking down the intervention (emergency anaesthesia and tracheal intubation) into its core components, we identified the preparation stage to be critical in determining both the safety of the procedure and the time required to perform the intervention.



Key area where most gains could be made was the improvement of Preparation of equipment and drugs
Our aim was to develop a product that would be clinically meaningful, this being to reduce Intervention Time, reduce Error Rate and Cognitive Load of the operator / assistant. This is where the value lies, and how the concept of SCRAM™ was born.
Value lies in the ability to make a clinically meaningful impact
SCRAM™ (Structured CRitical Airway Management), invented by Paul Swinton and Neil Sinclair, was designed and developed to improve the time and safety of the delivery of pre-hospital emergency anaesthesia and tracheal Intubation. Over the past five years, as the community of clinicians using SCRAM™ in both the pre-hospital and hospital environments has grown, so has the diverse feedback, providing us with unique insight into how SCRAM™ is used by high performance teams within different clinical settings. This has enabled us to refine the design to meet the needs of the clinician, into what is now the current version.
| Design for High Performance
But, that’s only part of the story
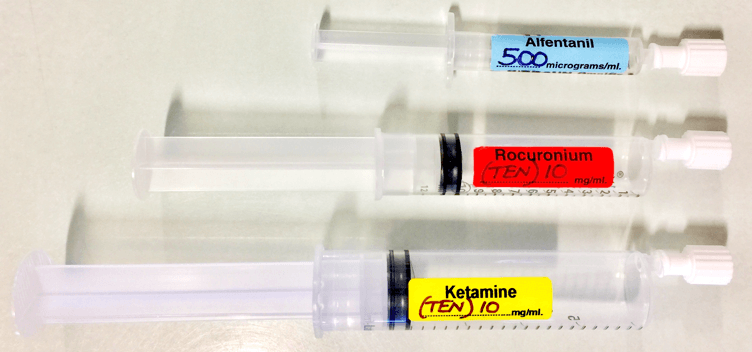
A significant proportion of time is spent preparing drugs, yet this is also where a significant proportion of errors occur. In a systematic review of drug administration error prevention during anaesthesia, Jensen et al. recommends “drugs should be presented in prefilled syringes (where possible) rather than ampoules (either for emergency drugs or in general)”7.
“Currently, there is wide variation in the way that pre-hospital services prepare drugs for Pre-hospital Emergency Anesthesia (PHEA), including using pharmacy-prepared drugs in pre-filled syringes, teams preparing the drugs at the start of the shift, drawing them up en route to an incident, and drawing them up on scene.
Syringes can be pre-prepared by the service or pharmacy. Individual services would need to consider the associated costs, waste, and shelf life of each method. The additional cost may, however, be offset by the accompanying reduction in the frequency of errors in preparing intravenous drugs and, more importantly, the iatrogenic harm and human cost of such errors8,9,10. Furthermore, the magnitude of the time reduction to administer the drugs for PHEA using pre-filled labelled syringes cannot be ignored”1.
| Simplify to amplify: Less load, more flow, fewer mistakes
Cognitive load and systemisation
Hick’s Law14 is a design principle used within the development of SCRAM™ to guide and adapt design and enhance performance.
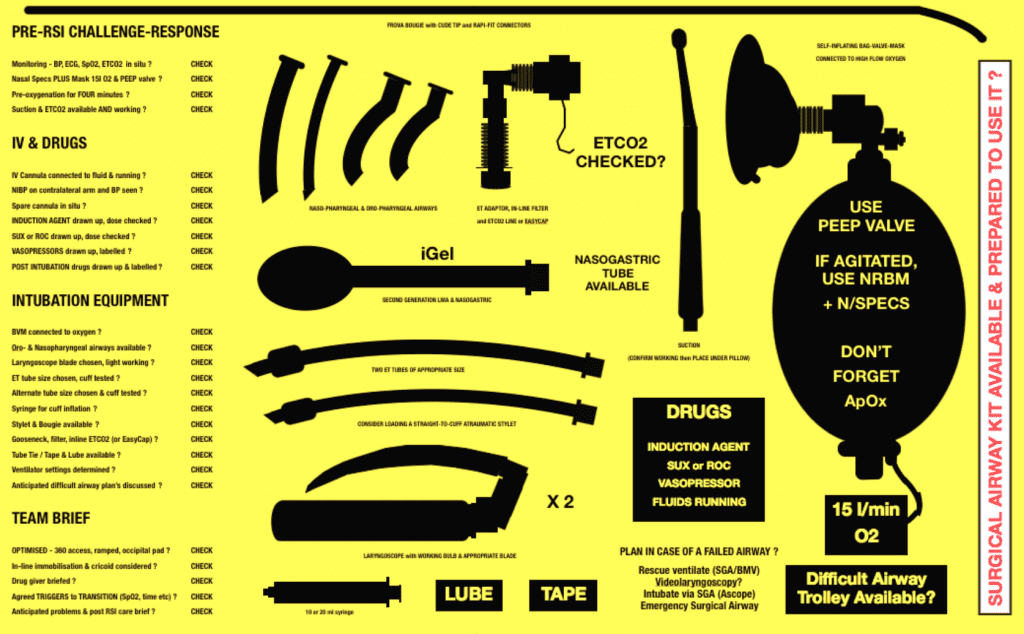
Planning and preparation of equipment are important components of emergency airway management. Poor planning and interrupted workflow at preparation (kit dump) stage of are significant contributors to morbidity and mortality,4 stressing the importance of systemisation, standardisation and cognitive offloading.1
Hick’s Law (or the Hick-Hyman Law) is named after a British and an American psychologist team of William Edmund Hick and Ray Hyman. In 1952, this pair set out to examine the relationship between the number of stimuli present and an individual’s reaction time to any given stimulus. As you would expect, the more stimuli to choose from, the longer it takes the user to make a decision on which one to interact with.14 So, the more choices you have or the harder the choices are, the longer it takes for you to make a decision and the more likely you’ll experience information overload. Which is of particular importance in the critical care high-stakes environment.
There are several ways of reducing cognitive load in critical situations, including the development of strategies such as briefings, flows (workflow patterns), and checklists and limiting the number of critical decisions that need to be made. The cognitive burden can potentially be further reduced by standardising the equipment and processes required for the intervention, for example by streamlining packaging or numbering various components sequentially. Such improvements could enhance patient safety by contributing to greater reliability, resilience and situational awareness.1,4
So, what is the SCRAM™ System?
The SCRAM™ System is a structured, reproducible approach to airway management, standardising, and optimally organising equipment and drugs prior to the procedure being required. The SCRAM™ System becomes a meaningful cognitive offloading tool, and facilitates airway planning by reducing the time to intervention, reducing error, standardising practice and promoting good governance.1 This is of particular importance now during the Covid-19 pandemic with increased cognitive demands of managing oneself, the team, the environment, the associated risks of error and time to intervention.
Community demand prompted further development of the SCRAM™ portfolio:
References:
- Swinton P, Corfield AR, Moultrie C, Percival D, Proctor J, Sinclair N, Perkins ZB. Impact of drug and equipment preparation on pre-hospital emergency Anaesthesia (PHEA) procedural time, error rate and cognitive load. Scandinavian journal of trauma, resuscitation and emergency medicine. 2018 Dec;26:82.
- Lockey D, Crewdson K, Davies G, Jenkins B, Klein J, Laird C, et al. AAGBI: safer pre-hospital anaesthesia 2017. Anaesth. 2017;72:379–90.
- Walz JM, Zayaruzny M, Heard SO. Airway management in critical illness. Chest. 2007 Feb 1;131(2):608-20.
- Schyma BM, Wood AE, Sothisrihari S, Swinton P. Optimising remote site airway management kit dump using the SCRAM bag—a randomised controlled trial. Perioperative Medicine. 2020 Dec;9(1):1-6.
- Durrand J, Batterham A, Danjoux G. Pre-habilitation (i): aggregation of marginal gains. Anaesthesia. 2014;69:403–6
- Cook T, Woodall N, Frerk C. Major complications of airway management in the UK: results of the fourth National Audit Project of the Royal College of Anaesthetists and the difficult airway society. Part 1: Anaesthesia. Br J Anaesth. 2011;106:617–31.
- Jensen LS, Merry AF, Webster CS, Weller J, Larsson L. Evidence-based strategies for preventing drug administration errors during anaesthesia. Anaesthesia. 2004;59:493–4.
- Pandit J, Andrade J, Bogod D, Hitchman J, Jonker W, Lucas N, et al. The 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: summary of main findings and risk factors. Br J Anaesth. 2014; 13:549–59.
- Webster CS, Merry AF, Ducat CM. Safety, cost and predrawn emergency drugs. Anaesthesia. 2001;56:799–20.
- Schnittker R, Marshall S, Horberry T, Young KL. Human factors enablers and barriers for successful airway management–an in‐depth interview study. Anaesthesia. 2018;16:980-989.
- Chrimes N, Bradley WP, Gatward JJ, Weatherall AD. Human factors and the ‘next generation ’airway trolley. Anaesthesia. 2018 Dec 14.
- Peterson GN, Domino KB, Caplan RA, Posner KL, Lee LA, Cheney FW. Management of the Difficult Airway A Closed Claims Analysis. The Journal of the American Society of Anesthesiologists. 2005 Jul 1;103:33-9.
- Credit for picture : Hawk T2 – Tim Davies https://fastjetperformance.com
Hick WE. On the rate of gain of information. Quarterly Journal of experimental psychology. 1952 Mar 1;4(1):11-26.